Innovative CAR T-Cell Therapy Shows Promise for Glioblastoma Treatment
Written on
Understanding Glioblastoma: A Deadly Brain Cancer
Glioblastoma, an aggressive form of brain cancer originating from star-shaped astrocyte cells, ranks as the most prevalent and ferocious primary brain tumor in adults. As an oncologist with three decades of experience, I still find the diagnosis unsettling. In 2015, I narrowly escaped a potentially life-threatening situation when a large pituitary tumor, possibly induced by prior radiation therapy, was confirmed not to be a brain cancer.
I don't refer to the typical pituitary tumors; I've undergone four surgeries related to mine. Recently, I was encouraged by early indications that a novel treatment approach could provide hope in this challenging context. This innovative strategy demonstrated remarkable responses in three patients suffering from recurrent glioblastoma, although sadly, all succumbed within approximately six months.
The Nature of Glioblastoma
Before delving into potential breakthroughs in treatment, it’s vital to understand the fundamentals of glioblastoma multiforme (GBM). GBM is a malignant tumor that arises from the proliferation of cells in the brain or spinal cord. This aggressive cancer not only proliferates swiftly but also invades and destroys healthy surrounding tissues.
Glioblastoma tends to occur more frequently in older adults and is more prevalent in men. Symptoms typically encompass worsening headaches, nausea, vomiting, blurred or double vision, persistent drowsiness, personality shifts, and seizures. Unfortunately, while treatments can slow the progression of the disease and alleviate symptoms, a cure for glioblastoma remains elusive.
The Challenges of Treatment
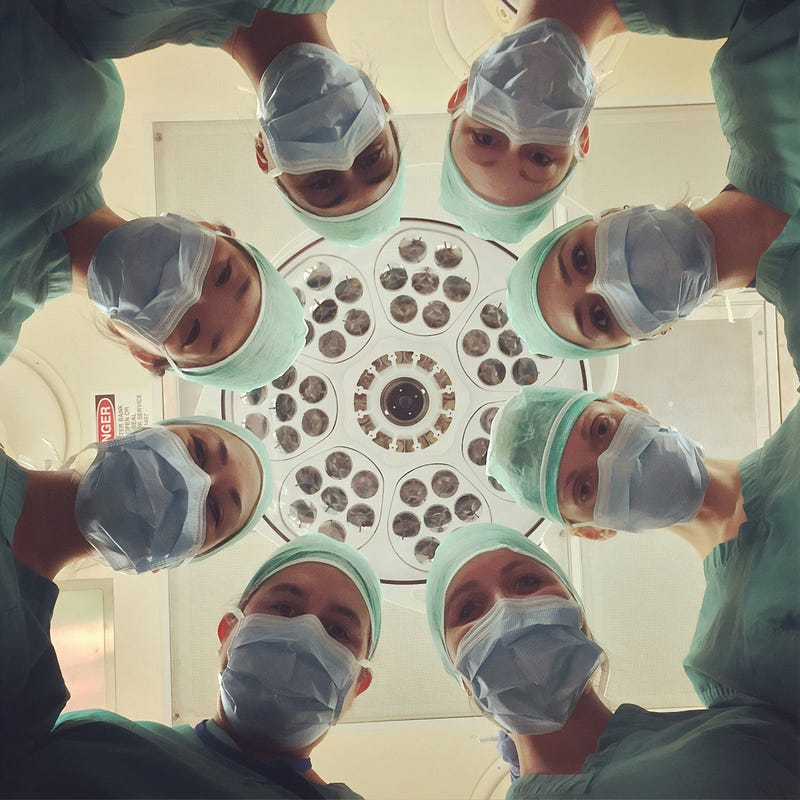
Current treatment modalities, such as surgery, radiation therapy, chemotherapy, and electromagnetic field therapy, often result in a poor prognosis for GBM patients. Although these interventions can prolong survival, they do not cure the disease.
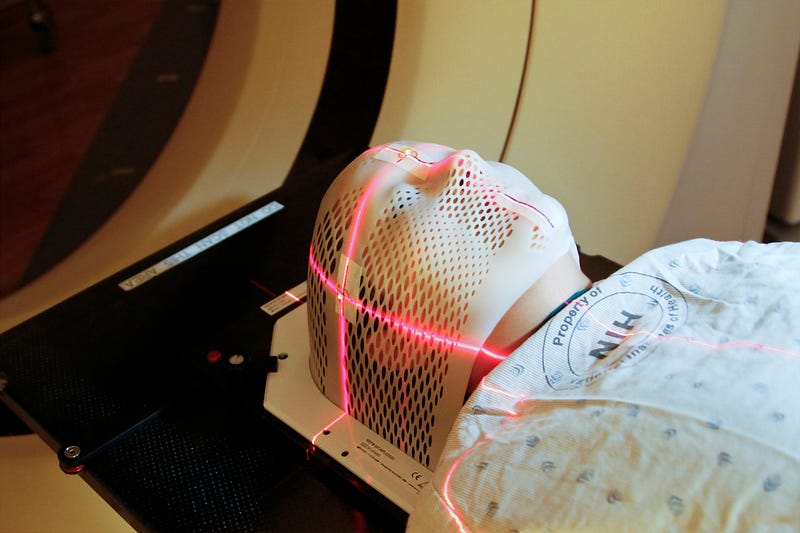
Historically, cancer treatment revolved around surgery, chemotherapy, and radiation. However, a new era of targeted therapies is reshaping the landscape of cancer treatment. Drugs like Gleevec and Herceptin specifically target alterations in cancer cells, benefiting many patients. Additionally, immunotherapy—which enhances the immune system's ability to combat cancer—has shown remarkable success in shrinking tumors and achieving long-term remission in some cases.
Innovative Approaches: CAR T-Cell Therapy
One emerging form of immunotherapy is CAR T-cell therapy, or chimeric antigen receptor T-cell therapy. This method employs the body’s immune system to specifically target and eliminate cancer cells.
Here’s a brief overview of the CAR T-cell therapy process:
- T-Cell Collection: Physicians extract T-cells, a type of white blood cell crucial for identifying and attacking abnormal cells, from the patient's blood.
- Genetic Engineering: In the laboratory, T-cells are modified to express chimeric antigen receptors (CARs) on their surfaces, enabling them to recognize and bind to specific proteins on cancer cells.
- Expansion of CAR T-Cells: The engineered T-cells are multiplied to create a substantial population ready to combat cancer.
- Infusion into the Patient: The activated CAR T-cells are then reintroduced into the patient's bloodstream to seek out and destroy cancer cells.
- Immune Response: Upon binding to cancer cells, CAR T-cells initiate a robust immune response that can lead to the direct destruction of the tumor and recruit additional immune cells to assist in the fight.
- Monitoring for Recurrence: Some CAR T-cells persist in the body, serving as sentinels that can quickly react if cancer cells reappear.
This pioneering therapy offers hope for patients dealing with certain advanced or treatment-resistant cancers.
Recent Advances in CAR T-Cell Therapy for Glioblastoma
Researchers at Massachusetts General Hospital have recently explored a novel approach to CAR T-cell therapy.

By engineering CAR-TEAM cells, the research team aimed to target mixed cell populations within tumors. In a phase 1 clinical trial involving patients with recurrent glioblastoma, initial results were promising.
Exciting Results: A Glimpse of Hope
The preliminary findings from the first three patients were astonishing, with rapid responses observed within days. Dr. Stephen J. Bagley, MD, MSCE, chief of neuro-oncology at Penn Medicine, expressed surprise at the outcomes, stating, "These results exceeded our expectations." However, translating these results into significant clinical benefits proved challenging.
Brain Cancer Breakthrough: New Clinical Trial Tests Direct-to-Tumor Method - This video discusses a new clinical trial that tests a novel method for delivering treatments directly to tumors, showcasing its potential impact on brain cancer therapies.
Balancing Expectations with Reality
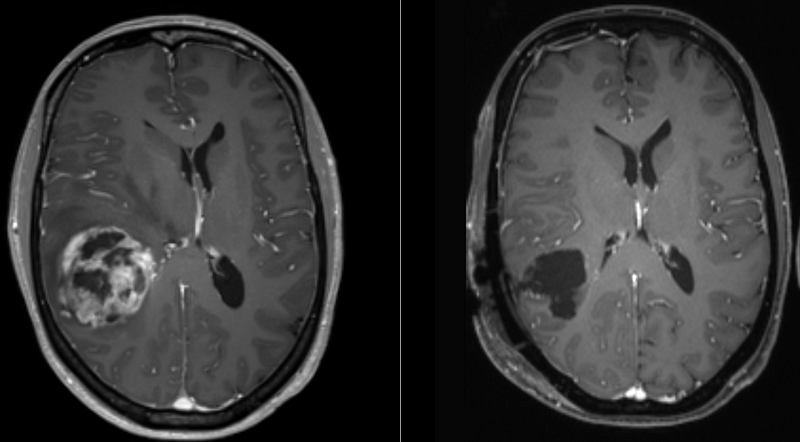
Using a new delivery mechanism and a dual-targeting strategy, the novel approach yielded rapid results. Among the clinical outcomes observed:
- Patient #1 experienced tumor regression for 33 days.
- Patient #2 passed away due to hydrocephalus, unrelated to treatment, after two months of stable disease.
- Patient #3 maintained stability for seven months.
- Patient #4 enjoyed three months of tumor stability.
- Patients #5 and #6 exhibited one month of stability at the time of reporting.
Despite the rapid outcomes, all patients experienced side effects, particularly neurotoxicity, within 72 hours post-treatment.
Moderate side effects included fatigue, skin issues, loss of appetite, reduced oxygen levels, muscle weakness, and dips in certain blood counts.
Looking Ahead: Future Directions
Researchers are planning to enroll 18 patients in an upcoming trial to assess how long the responses last and their impact on survival. Additionally, they aim to understand why CAR T-cell therapy is more effective for some patients than others. The ability to extract spinal fluid serially enables rapid biomarker analysis.
Conclusion: A Hopeful Future
I remain optimistic that this pilot study could enhance the management of aggressive brain tumors. Should ongoing research yield improved outcomes, there may be potential to apply CAR T-cell therapy earlier in the treatment process. Targeting multiple cellular pathways with localized delivery could also advance the treatment of other solid tumors.
Northwestern Medicine Achieves Breakthrough in Brain Cancer Treatment - This video highlights the groundbreaking advancements made by Northwestern Medicine in treating brain cancer, providing insights into their innovative strategies.
Thank you for exploring “Innovative CAR T-Cell Therapy Shows Promise for Glioblastoma Treatment.”